SILVER SPRING, Md. and RESEARCH TRIANGLE PARK, N.C., April 23, 2020 /PRNewswire/ -- United Therapeutics Corporation (Nasdaq: UTHR) today detailed recent publications on Orenitram® (treprostinil) Extended-Release Tablets, which provide additional evidence of the beneficial treatment effect in patients with pulmonary arterial hypertension (PAH).
Orenitram was originally approved by the U.S. Food and Drug Administration (FDA) in 2013, with a label indicating that it improves PAH patients' exercise capacity when used as a monotherapy. As a result of the FREEDOM-EV clinical study, the labeling was updated by the FDA in October 2019 to indicate that Orenitram delays disease progression when used in conjunction with an oral background PAH therapy.
The recent publications add further to the evidence showing the benefits of treatments with Orenitram in PAH patients:
- Data from the FREEDOM-EV hemodynamic sub-study showing that Orenitram significantly improved key hemodynamic parameters, including pulmonary vascular resistance (20% reduction), cardiac output (19% increase), and cardiac index (17% increase), at a median week 24 dose of 5.5 mg three times daily were recently presented at the Pulmonary Vascular Research Institute (PVRI) 14th Annual World Congress on Peripheral Vascular Disease (PVD).1
- Analyses of the FREEDOM-EV study showing that Orenitram significantly improved patient risk status assessed by two different methodologies (REVEAL 2.0 and French noninvasive), which can be predictor of clinical worsening and survival, were accepted for presentation at the American Thoracic Society (ATS) 2020 International Conference.2,3
- A retrospective database analysis of U.S. health insurance claims concluding that treatment with selexipag was associated with 67% higher PAH-related patient healthcare costs compared to Orenitram despite similar adherence, persistence, and rate of PAH-related hospitalizations was recently published in the journal Drugs – Real World Outcomes.4,5,6 (Comparison of products does not imply clinical comparisons of safety or efficacy.)
"FREEDOM-EV demonstrated that Orenitram treatment not only delays disease progression, but also leads to durable improvement in clinically relevant components of risk, including six-minute walk distance, NT-proBNP, and functional class," said Andrew Nelsen, PharmD, United Therapeutics' Head of Global Medical Affairs. "These additional analyses, coupled with the hemodynamic improvements, should bolster PAH physician confidence in treatment."
"Data from the FREEDOM-EV study have resonated well with PAH providers and payers," said Michael Benkowitz, President and Chief Operating Officer of United Therapeutics. "We are pleased to share these additional data, which we believe distinguishes Orenitram in the oral prostacyclin drug class and strengthens its value proposition to physicians, payers and patients. We appreciate the investigators and patients who participated in these studies."
Newly published data are summarized below. Please refer to the respective publications for further information.
Significant Impact on Hemodynamics – Data from the FREEDOM-EV Study
FREEDOM-EV was a phase III, international, multi-center, randomized, double-blind, placebo- controlled, event-driven study of Orenitram in patients with PAH receiving background oral monotherapy (N=690).7,8 Orenitram decreased the risk of adjudicated clinical worsening events by 25% compared to placebo (hazard ratio: 0.75; p=0.039). These results were largely driven by a 61% decrease in the risk of disease progression compared to placebo (hazard ratio: 0.39; p=0.0002).
The hemodynamic sub-study included 61 patients who volunteered for right heart catheterization at baseline and study Week 24.1,9 Patients were predominantly female (75%) and received background phosphodiesterase type 5 inhibitor, soluble guanylate cyclase stimulator (85%), or endothelin receptor antagonist (15%) therapy.
At Week 24, the median (interquartile range) Orenitram dose achieved was 5.5 (3.5, 6) mg three times daily (TID). Treatment with Orenitram resulted in significant changes in hemodynamic parameters at Week 24, including a:
- 20% reduction in pulmonary vascular resistance (PVR; p=0.0241);
- 21% reduction in pulmonary vascular resistance index (PVRI; p=0.0295);
- 19% increase in cardiac output (CO; p=0.0051);
- 17% increase in cardiac index (CI; p=0.0128); and
- 13% increase in stroke volume (SV; p=0.043).
There were no significant changes in other hemodynamic parameters, including mean right atrial pressure (RAPm), pulmonary artery wedge pressure (PAWPm), pulmonary artery pressure (PAPm), or heart rate (HR) between the Orenitram and placebo groups. Data set are represented in the table below.
The most common adverse reactions reported were consistent with the parent study and included headache, diarrhea, flushing, nausea, and vomiting.
Data are limited by the relatively small sample size compared to the parent study (61 patients v. 690 patients). Authors note that baseline patient characteristics were similar; however, median Orenitram dose achieved was higher in hemodynamic sub-study patients (5.5 mg TID vs. 3.56 mg TID, overall).
Significant Impact on Risk – Data from the FREEDOM-EV Study
Orenitram demonstrated a robust impact on key measures of disease status in the FREEDOM-EV study, including functional class, NT-proBNP levels, and French noninvasive risk profile.7,8 Those treated with Orenitram exhibited a statistically significant improvement in French noninvasive risk profile compared to placebo through study Week 60. This is of particular note, as despite seemingly balanced characteristics, placebo-assigned participants were found to be at lower risk at baseline (p=0.002).
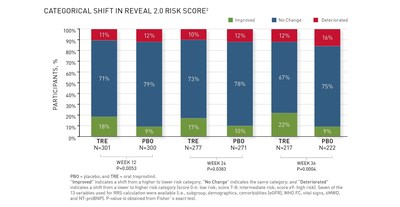
Thus, a post-hoc analysis of FREEDOM-EV was performed to determine the impact of Orenitram on the REVEAL 2.0 risk score (RRS).2 At baseline, 53%, 26%, and 21% of Orenitram subjects were in low (score 0-6), intermediate (score 7-8), and high-risk (score ≥9) categories, respectively, compared with 61%, 21%, and 18% of placebo subjects, respectively. The baseline RRS distribution was not statistically different between groups (p=0.0831), although mean scores between the groups were (6.3 Orenitram vs. 5.83 placebo; p=0.0107). Compared to baseline, there was a statistically significant improvement in RRS category in those treated with Orenitram compared to placebo through Week 36 (see figure, beyond Week 36 not presented). At Week 36, the mean RRS in participants treated with Orenitram decreased by 0.61, compared to a decrease of 0.01 in participants treated with placebo (mean difference: -0.599; p=0.002).
To further assess the impact of the imbalance in patient risk in FREEDOM-EV, primary endpoint results were alternatively adjusted by baseline risk score.3 That is, the primary endpoint was corrected for the imbalance in baseline patient risk. Adjusting the primary endpoint analyses by baseline risk score magnified the treatment effect already observed in the pre-specified analysis (a 25% reduction in clinical worsening with Orenitram; hazard ratio: 0.75; p=0.039). Adjusting by the French noninvasive methodology, Orenitram was found to decrease the risk of clinical worsening events by 39% compared to placebo (hazard ratio: 0.61; p=0.0006). Adjusting by RRS (as a continuous variable), Orenitram decreased the risk of clinical worsening events by 33% compared to placed (hazard ratio: 0.67; p=0.0047).
The authors comment that risk scores appear to be a robust stratification tool and may be more sensitive for detecting treatment effects than traditional stratification factors.
Assessment of patient risk status via French noninvasive methodology was prespecified as an exploratory analysis in the FREEDOM-EV statistical analysis plan. Additional evaluations on patient risk were conducted post-hoc and should be regarded with appropriate caution.
Cost Effectiveness – Data from a U.S. Health Insurance Claims Study
A total of 256 patients with PAH receiving oral prostacyclin therapy were included in this retrospective database analysis (130 Orenitram and 126 selexipag patients).4,5,6 Various outcomes were evaluated over a six-month follow-up period, including adherence to treatment, persistence on treatment, all-cause and PAH-related hospitalizations, as well as healthcare costs.
Adherence, persistence, and hospitalization outcomes were comparable between patient groups. Treatment adherence was measured using the medication possession ratio (MPR) and the proportion of days covered (PDC). Mean MPR was higher for Orenitram patients (p=0.039), but there were no significant differences in the proportion of patients with ≥80% mean MPR, mean PDC, or ≥80% PDC between groups. Also, there was no significant difference between groups in the proportion of patients persistent on treatment, when discontinuation was defined as a gap in treatment of either ≥30 or ≥60 days. Mean number of all-cause outpatient visits was higher with Orenitram (p<0.001). However, there was no significant difference between groups in number of all-cause and PAH-related hospitalizations, length of hospital stay, or number of emergency department visits.
Healthcare costs differed significantly between the treatment groups. Treatment with selexipag was associated with 51.4% higher mean total healthcare costs compared to Orenitram (mean difference of $73,680; p<0.05). This finding was primarily driven by significantly lower pharmacy costs with Orenitram. Furthermore, treatment with selexipag was associated with 66.9% higher PAH-related mean total healthcare costs compared to Orenitram (mean difference of $75,183; p<0.05). Results were again primarily driven by significantly lower pharmacy costs with Orenitram.
The authors acknowledge the relatively small sample size included in the analysis and various health insurance claims database limitations, including inability to ascertain patient PAH disease severity, whether patients take medication as prescribed, and medication dose changes.
About FREEDOM-EV
FREEDOM-EV was a phase III, international, multi-center, randomized, double-blind, placebo- controlled, event-driven clinical worsening study of oral treprostinil in patients with PAH receiving background oral monotherapy (a phosphodiesterase type 5 inhibitor, an endothelin receptor antagonist, or a soluble guanylate cyclase stimulator).7 The primary endpoint of this study was met, as Orenitram decreased the risk of adjudicated clinical worsening events by 25% compared to placebo (p=0.039). These results were largely driven by delay in disease progression; Orenitram decreased the risk of disease progression by 61% compared with placebo (p=0.0002).
Global enrollment was completed in December 2017 with a total of 690 patients. Patients were randomized 1:1 to receive three daily doses of Orenitram or placebo. This event-driven study was conducted in 152 centers from 23 countries in North and Latin America, Europe, and Asia- Pacific, with 214 patients having an adjudicated clinical worsening (morbidity or mortality) event: death, hospitalization due to worsening of PAH, initiation of inhaled or infused prostacyclin treatment for PAH, disease progression, or unsatisfactory long-term clinical response. Disease progression was defined as a decrease in six-minute walk distance (6MWD) by ≥15% and an increase in functional class or the appearance or worsening of right-heart failure. Dosing in FREEDOM-EV was initiated at 0.125 mg three times daily (TID) and increased to a maximum of 12 mg TID. This event-driven study was designed to demonstrate a prolongation of time to the first adjudicated clinical worsening event for patients treated with Orenitram compared with placebo and to further establish the safety of Orenitram in PAH patients. Investigator-reported clinical worsening events were adjudicated by an independent committee blinded to study treatment. Mortality was analyzed at the end of randomized treatment and study closure, which included open-label treatment. Vital status was assessed at six-month intervals for consenting individuals who discontinued participation.
Secondary Endpoints
Secondary endpoints included changes from baseline in 6MWD, Borg dyspnea score (shortness of breath test), functional class, NT-proBNP levels, and combined 6MWD and Borg dyspnea score. Secondary endpoint data, which are not included in the FDA-approved labeling, are summarized below:
- Change in 6MWD: The median 6MWD trended toward improvement at week 24 (Hodges-Lehmann treatment estimate: 7 meters). Median 6MWD improved with Orenitram at weeks 36 (13 meters) and 48 (21 meters) compared to placebo. Six-minute walk distance at week 24 was not significantly different from placebo.
- Change in Borg dyspnea score and World Health Organization (WHO) functional class: When classified categorically as 'improved', 'no change', or 'deteriorated', participants in the Orenitram group exhibited a significantly positive shift in Borg dyspnea score and WHO functional class compared to placebo at weeks 24, 36, and 48.
- Change in NT-proBNP levels: NT-proBNP levels were significantly improved with Orenitram at weeks 24 and 36. Per protocol, NT-proBNP was not assessed at week 48.
- Change in combined 6MWD and Borg dyspnea score: Combined 6MWD and Borg dyspnea score was significantly improved with Orenitram when assessed at week 24 compared to placebo.
Vital Status Sub-study
In FREEDOM-EV, vital status was collected throughout the study from patients who agreed to be followed. This included patients who discontinued early and those who transitioned to the open-label continuation study. When vital status was collected, cause of death was not specified.
Mortality was similar between Orenitram and placebo groups at the end of randomized treatment and the open label extension. However, in participants for which data are available (89%; unknown for 43 Orenitram and 31 placebo patients), Orenitram was associated with a 37% decreased risk of mortality compared with placebo at study closure. This mortality data is not reflected in the FDA-approved label, since it includes data accrued in the open-label extension study. Due to data collection limitations, data must be interpreted cautiously.
References
1. White RJ, Bohns Meyer GM, Pulido T, et al. Treatment with oral treprostinil improves hemodynamics in participants with PAH. Presented at: PVRI 14th Annual World Congress on PVD; January 30-February 2, 2020; Lima, Peru. Accessible at: https://pvrinstitute.org/en/professionals/learning/2020/2/15/97-treatment-with-oral-treprostinil-improves-hemodynamics-in-participants-with-pah/
2. Benza RL, Gomberg-Maitland M, Farber HW, et al. An analysis of FREEDOM-EV using the French noninvasive and REVEAL 2.0 risk stratification criteria. Accepted to: ATS International Conference; May 15-20, 2020; Philadelphia, PA. Accessible at: https://www.abstractsonline.com/pp8/#!/8998/presentation/17670
3. Benza RL, Gomberg-Maitland M, Farber HW, et al. The impact of stratification by baseline pulmonary arterial hypertension risk score – analysis from the FREEDOM-EV study. Accepted to: ATS International Conference; May 15-20, 2020; Philadelphia, PA. Accessible at: https://www.abstractsonline.com/pp8/#!/8998/presentation/16752
4. Dean BB, Saundankar V, Stafkey-Mailey D, et al. Medication Adherence and Healthcare Costs Among Patients with Pulmonary Arterial Hypertension Treated with Oral Prostacyclins: A Retrospective Cohort Study. Drugs – Real World Outcomes. 2020 Mar 6. Accessible at: https://doi.org/10.1007/s40801-020-00183-x
5. Dean BB. Healthcare costs lower with treprostinil versus selexipag for PAH. PharmacoEcon Outcomes News. 2020;849:12. Accessible at: https://link.springer.com/article/10.1007%2Fs40274-020-6663-2
6. Wexler M. Orenitram tablets more cost-effective than Uptravi as PAH treatment, study suggests. Pulmonary Hypertension News. March 20, 2020. Accessible at: https://pulmonaryhypertensionnews.com/2020/03/20/orenitram-tablets-more-cost-effective-than-uptravi-as-pah-treatment-study-suggests/
7. White RJ, Jerjes-Sanchez C, Bohns Meyer GM, et al. Combination therapy with oral treprostinil for pulmonary arterial hypertension. A double-blind placebo-controlled clinical trial. Am J Respir Crit Care Med. 2020 Mar 15;201(6):707-717. Accessible at: https://doi.org/10.1164/rccm.201908-1640OC
8. Bryson S. Orenitram slows PAH progression when used with other therapies, Phase 3 trial finds. Pulmonary Hypertension News. January 13, 2020. Accessible at: https://pulmonaryhypertensionnews.com/2020/01/13/orenitram-slows-pah-progression-when-used-with-other-therapies-phase-3-trial-finds/
9. Data on file. United Therapeutics Corporation. Research Triangle Park, NC.
About Orenitram
Indication
Orenitram is a prostacyclin mimetic indicated for treatment of pulmonary arterial hypertension (PAH; WHO Group 1), to delay disease progression and to improve exercise capacity. The studies that established effectiveness included predominately patients with WHO functional class II-III symptoms and etiologies of idiopathic or heritable PAH (66%) or PAH associated with connective tissue disease (26%).
Important Safety Information for Orenitram
CONTRAINDICATIONS
- Avoid use of Orenitram in patients with severe hepatic impairment (Child Pugh Class C) due to increases in systemic exposure.
WARNINGS AND PRECAUTIONS
- Abrupt discontinuation or sudden large reductions in dosage of Orenitram may result in worsening of PAH symptoms.
- The Orenitram tablet shell does not dissolve. In patients with diverticulosis, Orenitram tablets can lodge in a diverticulum.
ADVERSE REACTIONS
- In the 12-week, placebo-controlled, monotherapy study, and an event-driven, placebo- controlled, combination therapy study, adverse reactions that occurred at rates at least 5% higher on Orenitram than on placebo included headache, diarrhea, nausea, vomiting, flushing, pain in jaw, pain in extremity, hypokalemia, abdominal discomfort, and upper abdominal pain.
DRUG INTERACTIONS
- Co-administration of Orenitram and the CYP2C8 enzyme inhibitor gemfibrozil increases exposure to treprostinil; therefore, Orenitram dosage reduction may be necessary in these patients.
SPECIFIC POPULATIONS
- Animal reproductive studies with Orenitram have shown an adverse effect on the fetus. There are no adequate and well-controlled studies with Orenitram in pregnant women.
- It is not known whether treprostinil is excreted in human milk or if it affects the breastfed infant or milk production.
- Safety and effectiveness of Orenitram in pediatric patients have not been established.
- Use of Orenitram in patients aged 65 years and over demonstrated slightly higher absolute and relative adverse event rates compared to younger patients. Caution should be used when selecting a dose for geriatric patients.
- There is a marked increase in the systemic exposure to treprostinil in hepatically impaired patients.
Please see Full Prescribing Information and Patient Information at www.orenitram.com or call 1-877-UNITHER (1-877-864-8437).
About United Therapeutics
United Therapeutics Corporation focuses on the strength of a balanced, value-creating biotechnology model. We are confident in our future thanks to our fundamental attributes, namely our obsession with quality and innovation, the power of our brands, our entrepreneurial culture and our bioinformatics leadership. We also believe that our determination to be responsible citizens – having a positive impact on patients, the environment and society – will sustain our success in the long term.
Through our wholly-owned subsidiary, Lung Biotechnology PBC, we are focused on addressing the acute national shortage of transplantable lungs and other organs with a variety of technologies that either delay the need for such organs or expand the supply. Lung Biotechnology is the first public benefit corporation subsidiary of a public biotechnology or pharmaceutical company.
Forward-looking Statements
Statements included in this press release that are not historical in nature are "forward-looking statements" within the meaning of the Private Securities Litigation Reform Act of 1995. Forward-looking statements include, among others, statements regarding the impact of the FREEDOM-EV results on physicians, payers and patients, and the commercial potential for Orenitram. These forward-looking statements are subject to certain risks and uncertainties, such as those described in our periodic and other reports filed with the Securities and Exchange Commission that could cause actual results to differ materially from anticipated results. The forward-looking statements in this press release are qualified by the cautionary statements, cautionary language and risk factors set forth in our periodic reports and documents filed with the Securities and Exchange Commission, including our most recent Annual Report on Form 10-K, Quarterly Reports on Form 10-Q and Current Reports on Form 8-K. We claim the protection of the safe harbor contained in the Private Securities Litigation Reform Act of 1995 for forward-looking statements. We are providing this information as of April 23, 2020, and assume no obligation to update or revise the information contained in this press release whether as a result of new information, future events or any other reason.
ORENITRAM is a registered trademark of United Therapeutics Corporation.
Investor contact:
Dewey Steadman
ir@unither.com
(202) 919-4097
Media contacts:
Ryo Imai / Robert Flamm, Ph.D.
Burns McClellan
rimai@burnsmc.com / rflamm@burnsmc.com
(212) 300-8315 / (212) 300-8364
 View original content to download multimedia:http://www.prnewswire.com/news-releases/united-therapeutics-announces-additional-results-from-freedom-ev-study-showing-the-hemodynamic-and-risk-status-reduction-benefits-of-orenitram-treatment-in-patients-with-pulmonary-arterial-hypertension-301045819.html
View original content to download multimedia:http://www.prnewswire.com/news-releases/united-therapeutics-announces-additional-results-from-freedom-ev-study-showing-the-hemodynamic-and-risk-status-reduction-benefits-of-orenitram-treatment-in-patients-with-pulmonary-arterial-hypertension-301045819.html
SOURCE United Therapeutics Corporation